Investigators are always looking for new and innovative ways to treat cancer. This is a constantly and rapidly evolving field, with novel and experimental therapies such as cancer vaccines, CAR-T cells, and CRISPR frequently making the news. Recently, I came across preclinical research suggesting that targeting carbonic anhydrase 9 (“CA9” or “CAIX”), a hypoxia-induced pH regulatory enzyme in the tumor microenvironment (TME), can enhance the response to immune checkpoint inhibitors (published by a Canadian group here and here). While this exciting research needs confirmation in clinical trials, it has been known for a while that the TME can influence therapeutic responses and clinical outcomes. In this article, I briefly explore the concept of targeting the TME, with special focus on novel targets currently under investigation.
The “Tumor Microenvironment”
 The National Cancer Institute defines the TME as “The normal cells, molecules, and blood vessels that surround and feed a tumor cell.” They further go on to state that “A tumor can change its microenvironment, and the microenvironment can affect how a tumor grows and spreads.” The second part of this statement is especially important since a key feature of all ecosystems is that even a seemingly tiny alteration can cause dramatic reorganization of the entire system. In other words, just like reintroducing wolves into Yellowstone National Park had a ripple effect on the local ecosystem, deliberate alteration of the TME has the potential to augment the effects of other anti-cancer therapies and to slow or stop cancer progression.
The National Cancer Institute defines the TME as “The normal cells, molecules, and blood vessels that surround and feed a tumor cell.” They further go on to state that “A tumor can change its microenvironment, and the microenvironment can affect how a tumor grows and spreads.” The second part of this statement is especially important since a key feature of all ecosystems is that even a seemingly tiny alteration can cause dramatic reorganization of the entire system. In other words, just like reintroducing wolves into Yellowstone National Park had a ripple effect on the local ecosystem, deliberate alteration of the TME has the potential to augment the effects of other anti-cancer therapies and to slow or stop cancer progression.
Other sources (e.g. Sounnie and Noel, 2013) use stronger language when defining the TME, stating that many of the malignant features of cancer cells cannot be manifested without the interplay between these cells and the TME. That is, the cells of the TME (e.g. immune, angiogenic vascular, and lymphatic endothelial cells) actively contribute to tumor progression and/or metastasis.
Effects of the TME on Carcinogenesis and Drug Resistance
The TME can promote tumor growth in numerous direct and indirect ways. These include through increased angiogenesis, inflammation, cancer-associated fibroblasts (CAFs), changes in the extracellular matrix (ECM), altered immune activity due to high acidity etc. Moreover, the TME can also mediate drug resistance. For example, TME-mediated drug resistance can be induced by soluble factors secreted by the tumor or surrounding stromal cells, by increased adhesion of the tumor and stromal cells, or by altered expression of certain immune cells (e.g. tumor-associated macrophages). Developing novel drug combinations that can simultaneously target tumor cells and the TME may thus represent a way to overcome drug resistance. However, the large variety of stromal cells, the molecular complexity of the tumor stroma, and the similarity with normal tissue represent important challenges.
Targeting the Cellular Components of the TME
Angiogenesis
Traditionally, drugs targeting the TME have focused on the cellular components, including angiogenic endothelial and inflammatory cells. Notable antiangiogenic therapies include anti-VEGF and anti-VEGFR monoclonal antibodies (e.g. bevacizumab and ramucirumab) and other tyrosine kinase inhibitors targeting multiple pathways (e.g. sunitinib).
To date, there have been over 1000 clinical trials of antiangiogenic drugs worldwide. However, the survival benefits of many of these drugs have been modest. Further, they only work for certain tumor types and many patients eventually stop responding to the therapy.
These real-world results, along with discrepancies between preclinical and clinical data, suggest a possible role of microenvironmental defense mechanisms in treatment resistance. In fact, some authors have speculated that this may lead to a more aggressive and invasive tumor phenotype. Although this remains somewhat controversial, the challenges surrounding antiangiogenic therapies emphasize the need for predictive biomarkers and/or novel drug combinations with other antiangiogenics or drug classes.
Inflammation
It is known that chronic inflammation can promote cancer growth and survival. This is mediated by chronically activated polarized immune cells, which, in turn, produce various growth factors, chemokines, cytokines, and/or proteases. These factors then mediate tissue remodeling, angiogenesis, cell proliferation, and tumor spreading. In fact, in some cases such as chronic hepatitis B and C or H.pylori infection, the chronic inflammation is the direct cause of the cancer. This is not surprising considering that chronic inflammation associates with increased genomic damage, DNA synthesis, cell proliferation, angiogenesis, and invasion, as well as disruption of apoptosis and DNA repair. Moreover, tumorigenesis itself often induces activation of proinflammatory signalling pathways.
Considering the above, a number of drugs targeting various aspects of (tumor-associated) inflammation have been developed or are under investigation. Some of these, including steroids such as dexamethasone and prednisolone, have indeed been demonstrated to associate with improved efficacy of anti-cancer treatments. However, to date, the antineoplastic effects of other, more targeted, anti-inflammatory agents such as anti-IL-6 therapies have been modest at best.
Further, nonsteroidal anti-inflammatory drugs (NSAIDs) associate with a lower incidence and mortality of certain cancers (e.g. colorectal cancer) in patients with chronic inflammatory conditions. That said, with the exception of specific cyclooxygenase (COX) inhibitors, most NSAIDs are not specific and their gastrointestinal and cardiovascular side effects may prevent long-term administration.
Current Status of Anti-inflammatory Agents in Oncology
Overall, while there is strong preclinical evidence of the efficacy of anti-inflammatory drugs in cancer prophylaxis and therapy, clear clinical trial evidence is lacking for many novel agents. Especially, early trials of single agents have been disappointing, suggesting that the focus needs to shift to combination therapies to optimize efficacy and limit side effects.
Noteworthy, clinical research is ongoing on previously FDA-approved agents such as celecoxib. Additionally, the Repurposing Drugs in Oncology (ReDO) project is an interesting initiative looking at repurposing common drugs (including anti-inflammatory agents) for cancer prophylaxis and treatment.
Cancer-associated fibroblasts
 CAFs are a heterogeneous population of activated cells (mainly derived from fibroblasts) intricately associated with malignant tumor cells (see a detailed review of CAFs here). They are involved in cancer development and progression at all stages. These cells have multiple functions, including regulation of ECM turnover, epithelial differentiation, angiogenesis (through VEGF overexpression), and inflammation. They also regulate mesenchymal-epithelial cell interactions through the secretion of a number of growth factors such as IGF and EGF, as well as matrix metalloproteinases (MMPs). Taken together, these mechanisms help maintain an optimal microenvironment for cancer cell survival and proliferation and also mediate chemoresistance.
CAFs are a heterogeneous population of activated cells (mainly derived from fibroblasts) intricately associated with malignant tumor cells (see a detailed review of CAFs here). They are involved in cancer development and progression at all stages. These cells have multiple functions, including regulation of ECM turnover, epithelial differentiation, angiogenesis (through VEGF overexpression), and inflammation. They also regulate mesenchymal-epithelial cell interactions through the secretion of a number of growth factors such as IGF and EGF, as well as matrix metalloproteinases (MMPs). Taken together, these mechanisms help maintain an optimal microenvironment for cancer cell survival and proliferation and also mediate chemoresistance.
There is some early evidence that the molecules expressed on or secreted by CAFs may represent possible therapeutic targets. As one example, targeting fibroblast activation protein α (FAP) has been attempted in several early-stage trials. The results of recent preclinical studies (e.g. Duperret et al. 2018, O’Connell et al. 2019) are encouraging, although strong clinical trial evidence of a therapeutic benefit is still lacking.
Targeting the Non-cellular Tumor Microenvironment
The non-cellular TME includes physical and chemical parameters such as pH, oxygen tension, interstitial pressure, fluid changes, matrix geometry, electromagnetic fields, and ECM rigidity and density. All of these parameters have the potential to change the TME conditions to favor tumor progression. Accordingly, the non-cellular compartment functions as an important and dynamic regulator of cancer development, progression, and metastasis.
Extracellular Matrix Density and Stiffness
In the case of ECM density, its relationship with cancer can be demonstrated by the higher risk of breast cancer among women with high breast density. ECM deposition and stiffness enhance tumor progression through multiple mechanisms, including activation of integrin signalling and the ROCK pathway, development of focal adhesions, and actomyosin- and cytoskeletal-dependent cell contractility (summarized in more detail here).
The fact that increased stiffness is associated with advanced cancers makes it a promising prognostic marker and/or therapeutic target. In fact, not only stiffness but also its spatial distribution within the tumor and accompanying manifestations such as indistinct stromal boundary and changes in collagen fiber characteristics also represent potential biomarkers. Furthermore, ECM stiffness plays an important role in differentiation of stromal fibroblasts into CAFs.
Extracellular Matrix Reorganization
Through both biochemical and biophysical signalling, the ECM can modulate cell adhesion, migration, angiogenesis, and tissue remodelling, eventually leading to metastasis. Additionally, changes in ECM organization and/or activity can regulate cancer progression by clearing space for cell migration and modifying cell-to-matrix adherence. In the latter case, these changes are largely mediated by proteolytic enzymes such as serine proteases and MMPs, as well as growth factors and cytokines. As such, these enzymes represent promising targets, as well as predictive/prognostic biomarkers.
Matrix Metalloproteinases
In terms of MMPs, despite the large amount of preclinical evidence demonstrating roles in tumor invasion and metastasis, past clinical trials on MMP inhibitors have been unsuccessful in reducing tumor burden or improving survival. These agents also came with unexpected and often severe side effects. Winer et al. (2018) propose two main reasons for these disappointing results: (1) some MMPs have anti-tumor effects; therefore, the broad-spectrum MMP inhibitors used in early trials might have blocked these MMPs as well as those with pro-tumor effects. (2) MMPs are involved in the early stages of tumor progression whereas the MMP inhibitors were tested in patients with advanced disease. Thus, the authors concluded that, as more specific inhibitors are becoming available, MMP targeting should be reconsidered for cancer therapy in early-stage tumors.
Lysyl Oxidase
Lysyl oxidase (LOX) is another molecule of interest. It is a key enzyme in ECM remodelling and tissue tensile strength regulation. It also plays roles in gene transcription, motility/migration, and cell adhesion. In an in vivo PTEN-deficient breast cancer model, Chen et al. (2019) recently showed that genetic and pharmacologic inhibition of LOX markedly inhibited macrophage density and tumor growth in vivo. Other experimental studies (e.g. Cox et al. 2016) support these results.
pH
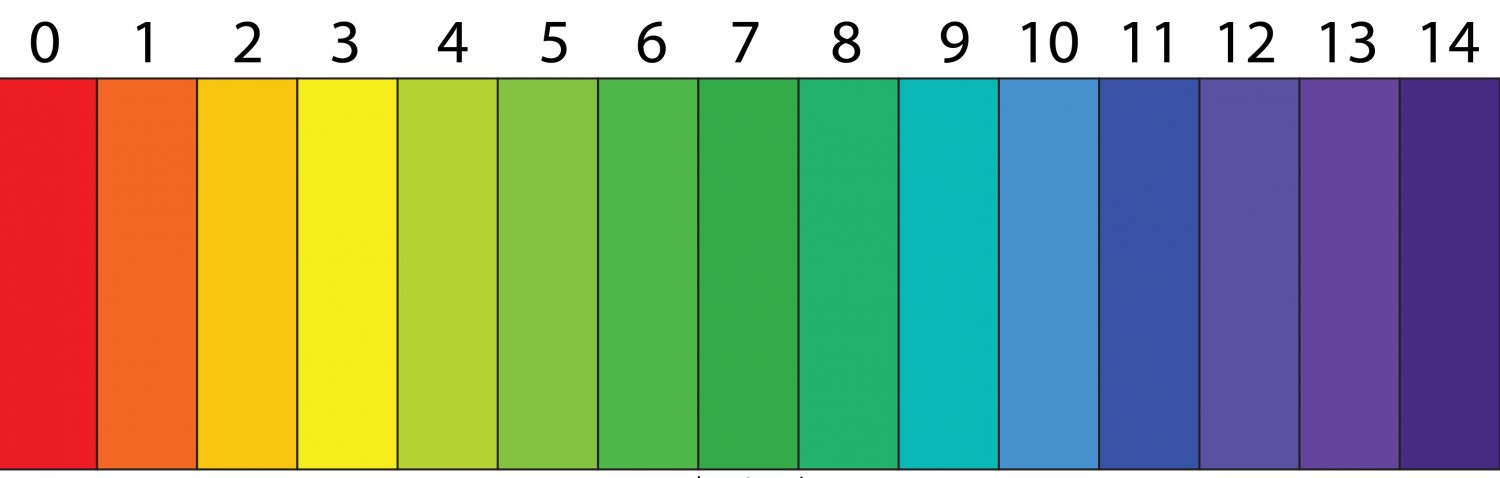
Aggressive cancers feature a rapid proliferation rate and exacerbated glycolysis. This results in excessive production of acids, consequently promoting immunosuppression and increased tumor aggressiveness, creating a positive feedback loop. In 2018, Kuchuk et al. showed that the pH-regulatory molecules CAIX, CAXII, and V-ATPase are overexpressed in the TME of hepatocellular carcinomas. Interfering with these pathways resulted in anti-tumor activity in their experimental model.
As mentioned above, a Canadian group recently published their preclinical data on targeting CAIX. The results of their study suggest that, in combination with immune checkpoint blockade, targeting CAIX is a potential therapeutic strategy for enhancing response and survival in patients with hypoxic solid malignancies.
Further, Kulshrestha et al. (2019) targeted V-ATPase in ovarian cancer and likewise found that its inhibition impaired ovarian cancer growth in vitro and in vivo by interfering with tumor acidification and activation of anti-tumor responses. Hence, targeting pH regulation is a promising strategy but time will tell whether the clinical trial results will mimic those from animal studies.
Next Steps for Pharma
The above is not a comprehensive overview by far. There are numerous other cellular and non-cellular targets in the TME under investigation. What we can say for sure though is that the TME is essential for cancer progression and metastasis. As such, it is important not to overlook it when planning your R&D pipeline. First, the optimal targets within the TME need establishment. Moreover, differences in the TME between different tumor types and cancer stages need to be clarified. Non-tumor cells are less likely to mutate and acquire treatment-resistance than their genetically unstable counterpart. Thus, they represent promising therapeutic targets in combination with treatments directly targeting the tumor cells. That said, the delicate balance between the TME’s pro- and anti-tumor activities makes this challenging.
 No matter how you choose to approach this, Impetus Digital is here to help! Online advisory boards with investigators or oncologists can help give you a better understanding of their perspectives and priorities, and clinical needs. Our best-in-class online platform, the Impetus InSite Platform®, can be used to co-create study protocols, peer-reviewed articles, abstracts, and posters with investigators or other key stakeholders. As a new feature, Impetus now also offers virtual “journal clubs” where your advisors can critique novel experimental or clinical studies. Furthermore, the platform can be used to facilitate communication and collaboration between investigators at multiple sites. The possibilities are endless!
No matter how you choose to approach this, Impetus Digital is here to help! Online advisory boards with investigators or oncologists can help give you a better understanding of their perspectives and priorities, and clinical needs. Our best-in-class online platform, the Impetus InSite Platform®, can be used to co-create study protocols, peer-reviewed articles, abstracts, and posters with investigators or other key stakeholders. As a new feature, Impetus now also offers virtual “journal clubs” where your advisors can critique novel experimental or clinical studies. Furthermore, the platform can be used to facilitate communication and collaboration between investigators at multiple sites. The possibilities are endless!
References
Chafe, S.C., McDonald, P.C., Saberi, S., et al. (2019). Targeting Hypoxia-Induced Carbonic Anhydrase IX Enhances Immune-Checkpoint Blockade Locally and Systemically. Cancer Immunol Res, 7, 1064-1078.
Chen, P., Wang, A., DePinho, R. (2019). Abstract A060: Targeting glioma-macrophage interplay via LOX in PTEN-deficient glioblastoma. Cancer Immunol Res February, 7(2 Supplement), A060.
Emon, B., Bauer, J., Jain, Y., et al. (2018). Biophysics of Tumor Microenvironment and Cancer Metastasis – A Mini Review. Computational and Structural Biotechnology Journal, 16, 279-287.
Hirata, E., Sahai, E. (2017). Tumor Microenvironment and Differential Responses to Therapy. Cold Spring Harbor perspectives in medicine, 7, a026781.
Jayson, G.C., Kerbel, R.,Ellis, L.M., et al. (2016). Antiangiogenic therapy in oncology: current status and future directions. The Lancet, 388, 518-529.
Kuchuk, O., Tuccitto, A., Citterio, D., et al. (2018). pH regulators to target the tumor immune microenvironment in human hepatocellular carcinoma. OncoImmunology, 7.
Kulshrestha, A., Katara, G.K., Ibrahim, S.A., et al. (2019). Targeting tumor associated pH regulators: Effective therapeutic strategy in ovarian cancer [abstract]. In: Proceedings of the American Association for Cancer Research Annual Meeting 2019; 2019 Mar 29-Apr 3; Atlanta, GA. Philadelphia (PA): AACR; Cancer Res, 79(13 Suppl), Abstract nr 106.
Mbeunkui, F., Johann Jr, D.J. (2009). Cancer and the tumor microenvironment: a review of an essential relationship. Cancer Chemother Pharmacol., 63, 571-582.
Rayburn, E.R., Ezell, S.J., Zhang, R. (2009). Anti-Inflammatory Agents for Cancer Therapy. Mol Cell Pharmacol., 1, 29-43.
Sounni, N.E., Noel A. (2013). Targeting the Tumor Microenvironment for Cancer Therapy. Clinical Chemistry, 59, 85-93.
Tao, L., Huang, G., Song, H., et al. (2017). Cancer associated fibroblasts: An essential role in the tumor microenvironment (Review). Oncology Letters, 14, 2611-2620.
Todoric, J., Antonucci, L., Karin, M. (2016).Targeting Inflammation in Cancer Prevention and Therapy. Cancer Prev Res., 9, 895-905.
Winer, A., Adams, S., Mignatti, P. (2018). Matrix Metalloproteinase Inhibitors in Cancer Therapy: Turning Past Failures Into Future Successes. Mol Cancer Ther., 17, 1147-1155.

